Abstract

Introduction: Thromboembolism is a well-recognized complication of patients with Philadelphia negative myeloproliferative neoplasms (MPN), potentially due to an endothelial injury caused by the activation of inflammatory cytokines. Among the MPNs, Polycythemia vera (PV) seemed to be the most associated with thrombotic events; however, essential thrombocytosis (ET) and primary myelofibrosis (PMF) are also at higher risk than the general population. Furthermore, arterial and venous thromboembolisms account for higher mortality in this population, causing approximately 45% of all disease-associated fatal events. Previous studies have explored the combined outcomes of venous thromboembolism (VTE) on MPN patients; however, none of them focused primarily on pulmonary embolism (PE). Therefore, we aimed to identify any potential demographic, socioeconomic, or clinical characteristics associated with PE in a large cohort of MPN patients admitted to US hospitals.
Methods: We inquired the Nationwide Inpatient Sample database to identify patients diagnosed with MPN from 2016-2018. We used the ICD-10 codes to identify the different types of MPN and compare patients with and without PE. The main outcomes were risk factors associated with PE and in-hospital mortality. We computed the chi-squared test and the Mann-Whitney U-test to compare the outcomes of patients with and without PE. We first conducted a univariate analysis. Clinically relevant characteristics and variables with a significant association (p<0.05) with the development of PE in the univariate analysis were considered for the multivariate model. We identified the risk factors associated with PE using multivariate logistic regression. Our analyses were conducted using Stata Statistical Software version 14 (StataCorp, College Station, TX).
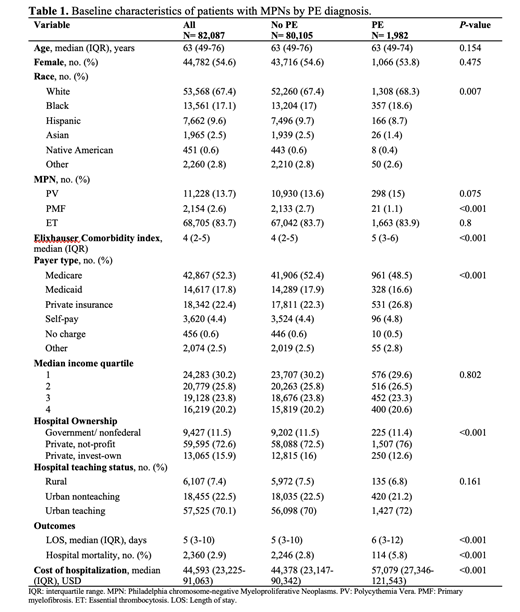
Results: Among 82,087 identified patients with MPN, most of them were white (67.4%), female (54.6%), and had a median age of 63 (IQR 49-76). Of them, 1982 (2.4%) had a PE event during admission. There were no significant differences in age and sex between PE patients and non-PE patients. While there were higher proportions of White (68.3% vs. 67.4%) and Black patients (18.6% vs. 17%) in the PE group, there was a lower proportion of Hispanics (8.7% vs. 9.7%; p=0.007). Patients with PE also had a higher median Elixhauser comorbidity index (5 vs. 4, p<0.001). There were fewer Medicare beneficiaries (48.5% vs. 52.4%) and a higher proportion of private insurance usage (26.8% vs. 22.3%; p<0.001) in the PE patients compared to those without PE. In the multivariate analysis, age, sex, race, or income quartile were not significantly associated with PE development. Compared to PV, patients with PMF had a protective effect for developing PE (OR: 0.35; CI 95%: 0.22-0.54). The comorbidities associated with higher odds for having a PE were coagulopathies (OR: 1.99; CI 95%: 1.71-2.30) and obesity (OR: 1.47; CI 95%: 1.29-1.67). See Table 1 for all the variables. Patients with PE had a higher length of stay (6 days vs. 5 days; p<0.001) and higher mortality than the non-PE group (6.1% vs. 2.8%; p<0.001).
Conclusions: In this large epidemiological study, we found that patients with MPN and PE had higher mortality than those without PE. Risk factors associated with the development of PE were concomitant obesity and coagulopathy. In addition to the known preventive therapies such as aspirin, phlebotomy, and cytoreductive agents, this study highlights the importance of controlling modifiable factors such as obesity in MPN patients. Future studies should confirm our findings and investigate strategies to prevention PE in this vulnerable population.
No relevant conflicts of interest to declare.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal